Bunion Deformities
Adult and Pediatric Deformity Correction
“I can’t change the direction of the wind, but I can adjust
my sails to always reach my destination – J. Dean
Let’s face it, we are often more like our parents than sometimes we wish to be, especially when it come to the shape and architectural makeup of our feet. This can especially be true when it comes to the formation of bunion deformities.
A bunion typically appears as a large and painful bump on the side of the great toe which is often exaggerated by the big toe leaning towards the second toe. If you suffer from this kind of deformity you are not alone, as this can affect up to 30% of adults. But what really causes this deformity and is there anything that can be done to change it for the better?
Download the Your Bunion Guide PDF
All about painful bunion deformities
 Although genetics do play an important role in our bone structure, it is not the only cause of bunions. While genetics often predispose us to the potential development of issues such as arthritis and deformities, bunion development is thought to be multi-factorial in nature.
Although genetics do play an important role in our bone structure, it is not the only cause of bunions. While genetics often predispose us to the potential development of issues such as arthritis and deformities, bunion development is thought to be multi-factorial in nature.
Environmental factors such as tight shoes, especially high heels or narrow dress shoes, the relaxation of ligaments as experienced during a pregnancy, or other structural abnormalities such as a flattened arch or inequality of the length of one’s legs can lead to instability of the great toe joint which can cause the toe to move out of its normal alignment.
Treatment of Bunion Deformities
Is pain from your bunion affecting your quality of life?
There are several ways to “grade” a bunion, but perhaps the most important question you should ask is what kind of impact your deformity is having on your desired lifestyle? If you do not have any pain associated with your bunion but you simply do not like the way it looks, then it is strongly recommended that you avoid surgical correction as this is only cosmetic in nature and there can be no guarantees that you will achieve your desired result without some sort of post-operative discomfort. On the other hand, if your deformity is having a significant impact on your quality of life by not allowing you to participate in activities that you normally like to do, or the discomfort causes you to no longer enjoy those activities, then you are likely a great candidate to correct the underlying issues and restore your quality of life.
Do I need surgery?
 While “fixing” a bunion deformity can only be accomplished through surgical reconstruction, there are several non-surgical options that are aimed to help to alleviate the symptoms associated with bunion deformities. These include wearing wider shoes with anatomic toe boxes, specialty shoe inserts or orthotics, bunion pads, and anti-inflammatory medication to reduce the swelling.
While “fixing” a bunion deformity can only be accomplished through surgical reconstruction, there are several non-surgical options that are aimed to help to alleviate the symptoms associated with bunion deformities. These include wearing wider shoes with anatomic toe boxes, specialty shoe inserts or orthotics, bunion pads, and anti-inflammatory medication to reduce the swelling.
Shoes such as Altra Running shoes have larger toe boxes to accommodate a foot that tends to be wider due to the bunion deformity. Other shoe manufactures, such as New Balance and Brooks Running also offer wider shoes that can accommodate special inserts or orthotic which can be really helpful.
 For more casual or dressier shoes you can look at Rockport for both men and women. Shoe brands that are historically known for comfortable and functional footwear include Finn Comfort, Ecco, Dansko, Naot, Birkenstock, Mephisto, Born, and Clarks.
For more casual or dressier shoes you can look at Rockport for both men and women. Shoe brands that are historically known for comfortable and functional footwear include Finn Comfort, Ecco, Dansko, Naot, Birkenstock, Mephisto, Born, and Clarks.
If you have tried a lot of these modifications and have not found the relief you were looking for, than you may be a good candidate for surgical correction of your deformity.
Are all bunion surgeries the same?
The answer is a resounding no. By now, you have probably heard horror stories from friends or family members who have had surgery on their feet only to experience a less than desirable outcome and leading them to the conclusion that they wished they had never had the surgery in the first place. There are a lot of methods and techniques that surgeons use to “fix” bunions, but not all of them are created equally leading to a relatively large variance in outcomes which can include a high level of failure/recurrence rates. However, if the “correct” procedure is selected based on your desired outcome and expectations, bunion correction can lead to very predictable, long-term, and desirable outcomes.

The good news is that there have been huge advancements in innovative surgical techniques as of more recent, which has helped both surgeons and patients find a much higher level of satisfaction with surgical intervention and significantly improved long-term outcomes.
In the past, most doctors would only “shave” the bump, which typically does nothing to address the underlying deformity and often results in a greater deformity. This is due to a common misconception that a bunion is simply an overgrowth of bone that can be shaved, when it is actually an angular deformity of the joint often caused by an instability in the middle of the foot which causes the toe to drift out of alignment.
Another method is to cut the metatarsal bone (Chevron Osteotomy) and shift it into a better position, but this too does not always fully restore the proper alignment and function to the great toe. There is a more advanced technique call a Lapidus Bunionectomy which has slowly become more of a “gold standard” in bunion correction due to the much lower recurrence/failure rate associated with it, but it is more technically challenging and several surgeons do not offer it. Dr. Perler has not only specialized in this technique, but he has helped in the innovation and development behind a couple of systems/devices which are now on the market which not only make it more reproducible, but help to allow for early weight-bearing, something that was not possible with the original version of this technique.
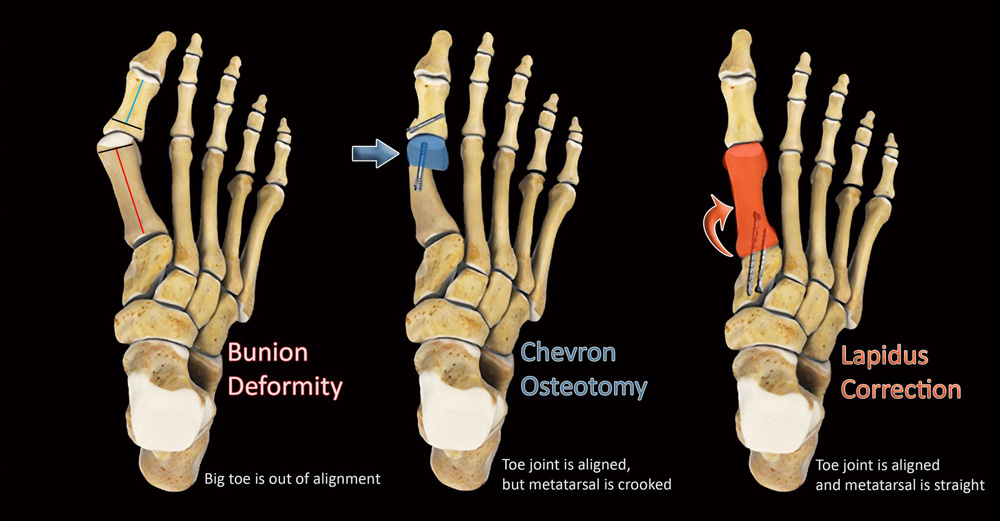
Chevron Osteotomy: The head of the metatarsal bone is cut and shifted into a corrected position achieving a corrected great toe joint but in exchange for a "crooked" metatarsal
Lapidus Correction: Swivels the entire metatarsal into a corrected position thus achieving both a bath a straight metatarsal bone and realigning the great toe joint.
New Innovations in Bunion Correction
As time has passed, more and more interest has been focused on innovation advancement in the field of foot and ankle surgery. In fact, for the last couple of years, foot and ankle has been the fastest growing segment in the orthopedic device industry with millions of dollars being allocated to research and development. What this has lead to is the release of multiple revolutionary new products that have significantly advanced the surgical approach to several techniques including bunion reconstruction.
One such advancement is in our understanding of the root cause of bunion formation which is actually joint mal-alignment due to instability and hypermobility of the great toe and the medial column of the foot (inner arch). For years, we have addressed bunion reconstruction as a two-dimensional problem. Our corrections have mainly been focused on bi-planar realignment of the great toe, whether it is with a traditional chevron osteotomy or a more advance Lapidus correction.
Click to learn more about each innovation.
Lapiplasty® 3D Bunion Correction™
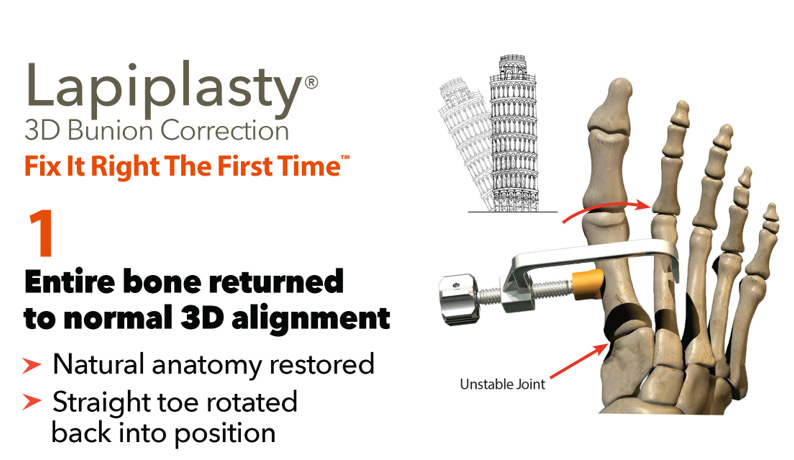
Treace Medical developed a new surgical technique along with several designer surgeons who realized that something was missing from traditional approaches and instead are now advocating for a three-dimensional or triplanar correction which improves upon the Lapidus with a technique called Lapiplasty.
With Lapiplasty, the first metatarsal is swiveled and rotated back in to proper alignment and a patented positioning jig is placed to dial in and fine tune the toe into the optimal position in all three planes.
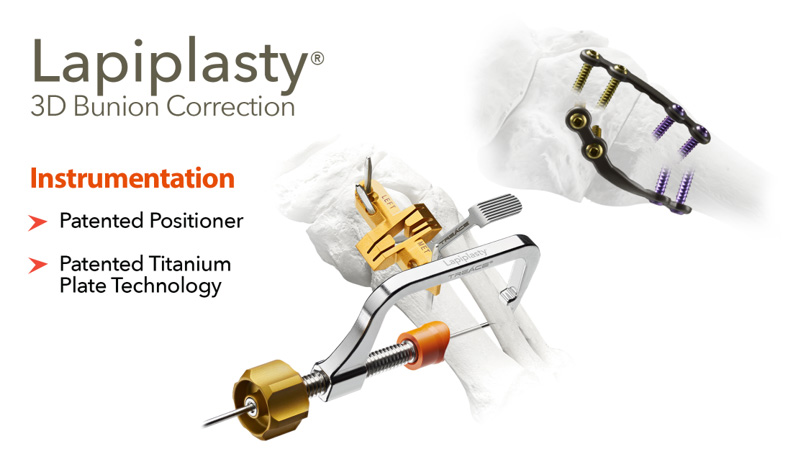
This significantly reduces the potential for under correction of the deformity, increases the accuracy and reproducibility of the technique, and greatly reduces the potential for a recurrence which is a major advantage of this technique
Learn More about Lapiplasty® 3D Bunion Correction™Bone Anchors
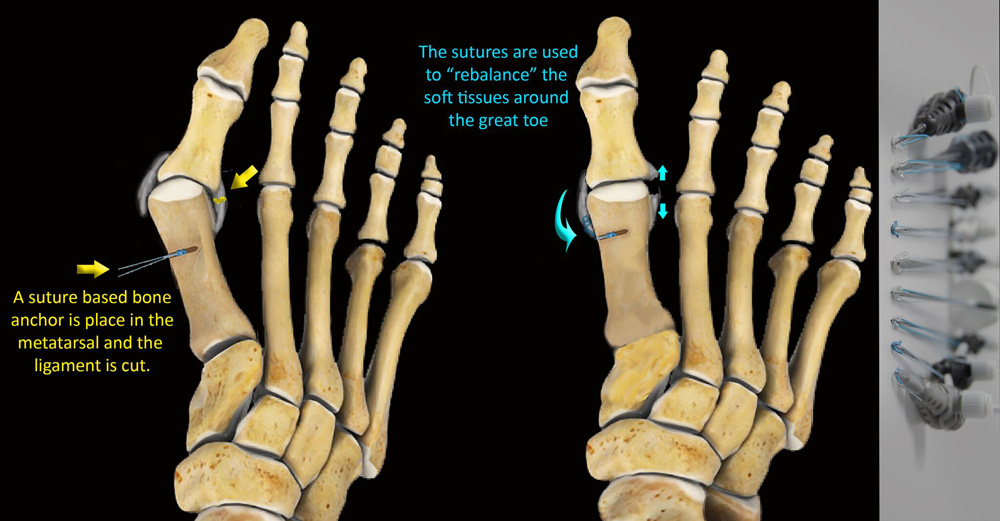
Another advanced technique that Dr. Perler has been instrumental in developing is the use of “bone anchors” to help rebalance the soft tissues around the great toe which get stretched over time and can cause further instability of the joint.
He has worked closely with several companies to develop recommended technique guides to help his peers utilize this unique innovation.
Unique Skin Closure Systems
For skin closure, Dr. Perler typically utilizes cutting-edge technology to give you an optimal outcome comes in the form of advanced materials for skin closure.
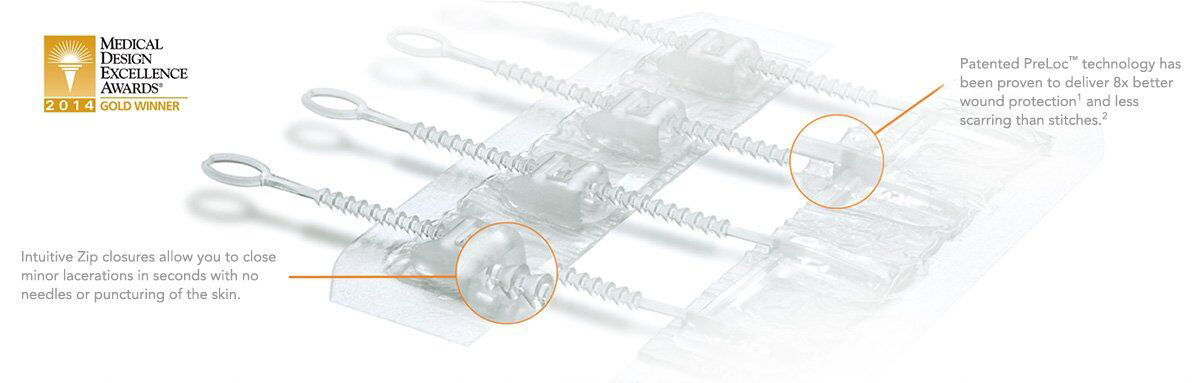
ZipLine Medical delivers innovative technology that improves the practice of medicine and enhances the patient recovery experience. They offer a sutureless skin closure system that works much like a shoe lace on a tennis shoe without the need for any skin punctures. Studies have shown that this allows the skin to heal quicker and allows for better vascularity at the incision site which aids in healing. It is also painless to remove.
Another great technology that Dr. Perler uses is a knotless suture called Quill that uses nano-technology to close the skin. It has tiny barbs and as it is weaved under the skin it helps to close the skin much like a zipper. It usually leaves very fine incision lines and when used, there is typically nothing to “remove” during the post-operative period since there are no knots and it is absorbable.

Recovering from Your Bunion Surgery
 Depending on the complexity of the surgery, either sedation and local anesthetic or general anesthetic is used during your procedure. Patients may go home the day of the surgery. The leg will be placed in a splint and should be kept elevated for the first two weeks. Care must be taken to not put any pressure on the backside of the heel. When you are elevating, place a pillow under the calf area and “float” the heel. Also, be sure to ice as directed. Although you will probably not feel the coolness through the dressings, the ice prevents the foot from overheating and keeps the swelling at a minimum. After a couple of weeks sutures are removed if external ones were used. A removable boot is then fitted and dispensed to you along with a special splint that will help to hold your toe in a corrected position while it heals. At this point you will be able to start to put weight on you foot with the use of your fracture boot starting at 30% of you body weight the first week and graduating to full weight-bearing over the following month. At week six, as long as your x-rays look good, you will be able to start to transition back into a “regular” shoe. Please know that you will likely have residual swelling for up to 6-8 months after your surgery. Also, at this time physical therapy may be recommended to help with scar tissue breakdown and range of motion of your great toe.
Depending on the complexity of the surgery, either sedation and local anesthetic or general anesthetic is used during your procedure. Patients may go home the day of the surgery. The leg will be placed in a splint and should be kept elevated for the first two weeks. Care must be taken to not put any pressure on the backside of the heel. When you are elevating, place a pillow under the calf area and “float” the heel. Also, be sure to ice as directed. Although you will probably not feel the coolness through the dressings, the ice prevents the foot from overheating and keeps the swelling at a minimum. After a couple of weeks sutures are removed if external ones were used. A removable boot is then fitted and dispensed to you along with a special splint that will help to hold your toe in a corrected position while it heals. At this point you will be able to start to put weight on you foot with the use of your fracture boot starting at 30% of you body weight the first week and graduating to full weight-bearing over the following month. At week six, as long as your x-rays look good, you will be able to start to transition back into a “regular” shoe. Please know that you will likely have residual swelling for up to 6-8 months after your surgery. Also, at this time physical therapy may be recommended to help with scar tissue breakdown and range of motion of your great toe.
Potential Complications
Complications may occur with any surgery and are not necessarily your fault, or the fault of your surgeon. Nonetheless, you should understand the risks. Modern surgical approaches typically involve a combination of procedures to realign the bone deformity using advanced technology as outlined above. These surgical treatments exceed a 95% percent success rate.
In addition to standard surgical risks such as infection, blood clots, risks of anesthesia, delayed wound healing, blood clot formation and nerve injury, additional risks may accompany procedures. For example, procedures that require bone healing (osteotomy, fusion) can result in a failure to properly heal the bones. The overall complication rates for these procedures are low.
These complications often can be prevented with proper wound care, full patient compliance in regard to weight bearing instructions and proper rehabilitation. Occasionally patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. There is also the possibility of either over or under correction of the deformity. Depending on any residual symptoms, a revision surgery may be required to further optimized your outcome, but this is not common thanks to the advancements in this particular surgery.

Frequently Asked Questions
Will surgical correction of my bunion deformity improve the cosmetic appearance of my foot?
Surgical correction of a bunion is aimed primarily at reducing pain and restoring function. Although surgery will likely improve the cosmetic appearance of the foot, it should not be one of the primary goals of treatment.
If I have my bunion corrected, is there any chance it will re-occur or come back?
This is a great question and really depends on the severity of your condition and what procedure was used to correct it. As stated above, there is a much higher recurrence rate associated with procedures that do not fully address the underlying cause of the deformity. With the advancement of the newer surgical techniques and methods of fixation, the recurrence rate is much lower when compared to even five years ago. If you do have any sort of recurrence, it should be mild and either non or minimally symptomatic.
What kind of activities will I be able to do after surgical correction?
This depends on the type and nature of procedures being performed. Following a successful surgery, you should be able to return to all pre-surgical activities with much less discomfort. Initially you will want to do lower impact activities such as cycling, swimming, exercise walking, and golfing which are all suitable for earlier stages of your recovery (six to twelve weeks). After 12 weeks you may resume higher impact activities such as plyometrics, running, jumping… and parachuting! Ideally, if your surgery has gone according to plan, your foot should no longer be a limiting factor in regards to your activities.
If you have any questions regarding your condition, please do not hesitate to reach out to us to make an appoinment so we can review and address any of your concerns. (727) 547-4700